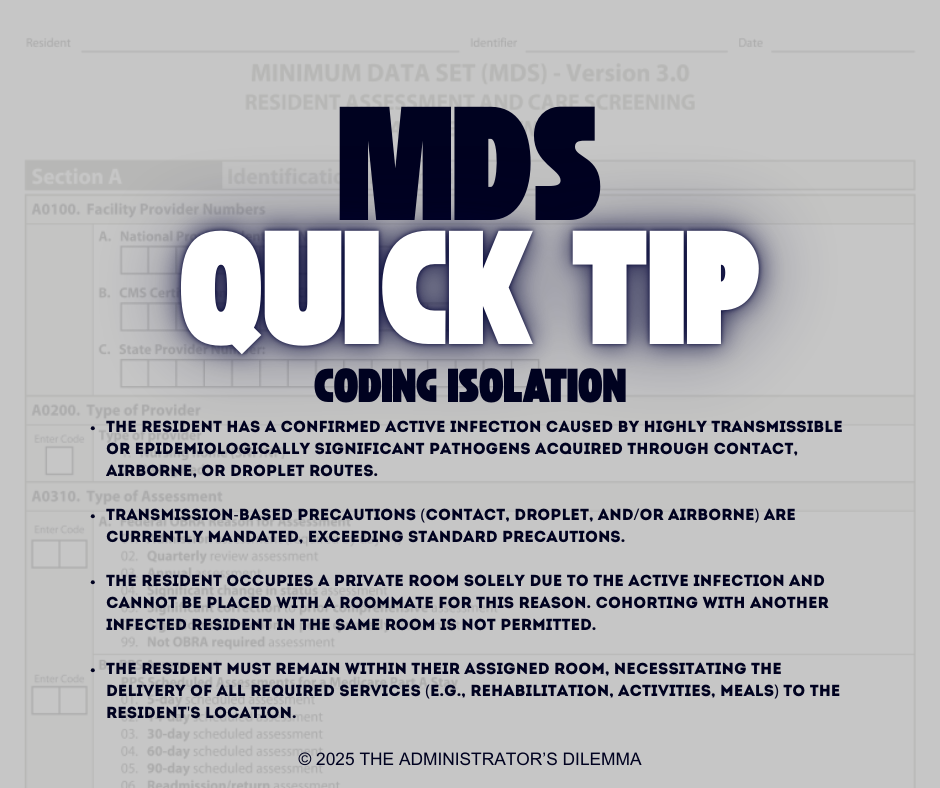
Understanding MDS Isolation Coding Criteria
Accurate MDS Isolation coding is a constant for long-term care administrators and staff. To help your team confidently apply these rules, we've broken down the strict four-part criteria you must meet to code for isolation.
4/11/20253 min read
Understanding Isolation Coding Criteria (RAI 3.0 User’s Manual - Effective October 2024)
To code isolation on the MDS assessment, ALL FOUR of the following criteria MUST be met simultaneously. If even one criterion is not met, you cannot code for isolation.
Active, Highly Transmissible Infection:
The resident must have an active infection. This means they are either symptomatic OR have a positive test AND are considered contagious.
The infection must be caused by a pathogen that is highly transmissible or epidemiologically significant (e.g., C. diff, Norovirus, Influenza, COVID-19, certain MDROs when transmission risk warrants it).
The transmission route must be physical contact, airborne, or droplet.
Key Exclusion: Do not code if the resident only has a history of an infection (like past MRSA or C. diff) but no current active symptoms or contagiousness. Also, infections like typical UTIs, encapsulated pneumonia, or contained wound infections generally do not meet this criterion.
Transmission-Based Precautions Required:
The precautions needed must be more than Standard Precautions.
This means Contact, Droplet, and/or Airborne precautions must be officially implemented according to established guidelines (like those from the CDC).
Key Exclusion: Do not code if only Standard Precautions (hand hygiene, gloves, potentially masks/gowns/eye protection used universally) are sufficient.
Resident is Alone in the Room (Strictly Single Occupancy):
The resident must be in a room by themselves specifically because of the active infection.
They cannot have a roommate, even if that roommate has the same infection (i.e., cohorting does not count for coding isolation under this item). The room must be designated as single occupancy due to the infection control need.
Resident Confined to Room:
The resident must remain in their room for the duration of the isolation period.
All services must be provided within the resident's room. This includes meals, activities, therapies (physical, occupational, speech), etc. They cannot leave the room to go to dining rooms, therapy gyms, or activity areas.
In Summary for Staff:
Before coding for isolation, ask these four questions:
Does the resident have a current, active infection known to spread easily through contact, droplets, or air? (Not just a history, not a contained UTI).
Are we using special Contact, Droplet, or Airborne precautions (beyond the standard ones)?
Is the resident completely alone in their room (no roommate at all)?
Is the resident required to stay in their room 24/7, with all services brought to them?
If the answer to ALL FOUR questions is YES, then you can code for isolation. If the answer to ANY question is NO, you cannot code for isolation, even if the resident is under some form of precautions or room restriction (like cohorting).
Important Considerations:
Resources: Use the referenced CDC and SHEA/APIC guidelines to determine appropriate precautions for specific infections.
2007 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html
SHEA/APIC Guideline: Infection Prevention and Control in the Long Term Care Facility http://www.apic.org/Resource_/TinyMceFileManager/Practice_Guidance/id_APIC-SHEA_GuidelineforICinLTCFs.pdf
Psychosocial Impact: Remember the manual acknowledges the negative psychosocial effects of isolation. While coding requires strict adherence to these criteria, always strive to balance necessary infection control with the resident's emotional and social well-being, providing in-room activities and support as much as possible.
Documentation: Ensure your documentation clearly supports why each of the four criteria is met when coding for isolation. This includes the type of infection, the specific transmission-based precautions ordered, the room status (single occupancy due to infection), and the plan for providing all services in the room.
Special Note: SCSA Review and Care Plan Modification
When a resident meets the criteria for coding isolation, facility staff must review the resident's overall status. Evaluate if the impact of the infection and the resulting isolation constitutes a "Significant Change in Status," potentially requiring a Significant Change in Status Assessment (SCSA). Refer to the RAI User's Manual Chapter 2, Section 2.6 for the specific SCSA criteria. Critically, even if an SCSA is not warranted, placing a resident under conditions that meet the isolation coding criteria will almost certainly necessitate modifications to the resident's plan of care to address changes in service delivery, monitoring, and psychosocial needs.
#TheAdministratorsDilemma #LNHA #NursingHomeAdmin #ExecutiveDirector #AIT #Leadership #LTC #SNF #SkilledNursing #NursingHome #Healthcare #HealthcareConsulting #Regulations #Operations #Reimbursement #MDS #Isolation #PDPM #RiskManagement #Compliance
Support
© 2025. All rights reserved.
Contact Us for Support
info@theadministratorsdilemma.com
Facing operational challenges in your nursing home? For administrators and operators, we provide personalized consulting and expert guidance to address your specific needs – from operational efficiency to clinical best practices and regulatory compliance. Let us help you develop a tailored strategy for achieving sustainable success and exceeding industry standards.